Endometriose - Die stille Pandemie in der Frauengesundheit
Endometriose ist eine komplexe Erkrankung, die durch das Wachstum von Endometriumgewebe außerhalb der Gebärmutter gekennzeichnet ist. Sie verursacht Symptome wie Schmerzen und Fruchtbarkeitsprobleme. Fortschritte in der Diagnostik und mögliche Autoimmunverbindungen bieten neue Behandlungsmöglichkeiten. Hormontherapie wird häufig eingesetzt, hat jedoch ihre Grenzen. Ernährung und Lebensstiländerungen können medizinische Behandlungen ergänzen. Caona Health bietet evidenzbasierte Lösungen für Endometriose.

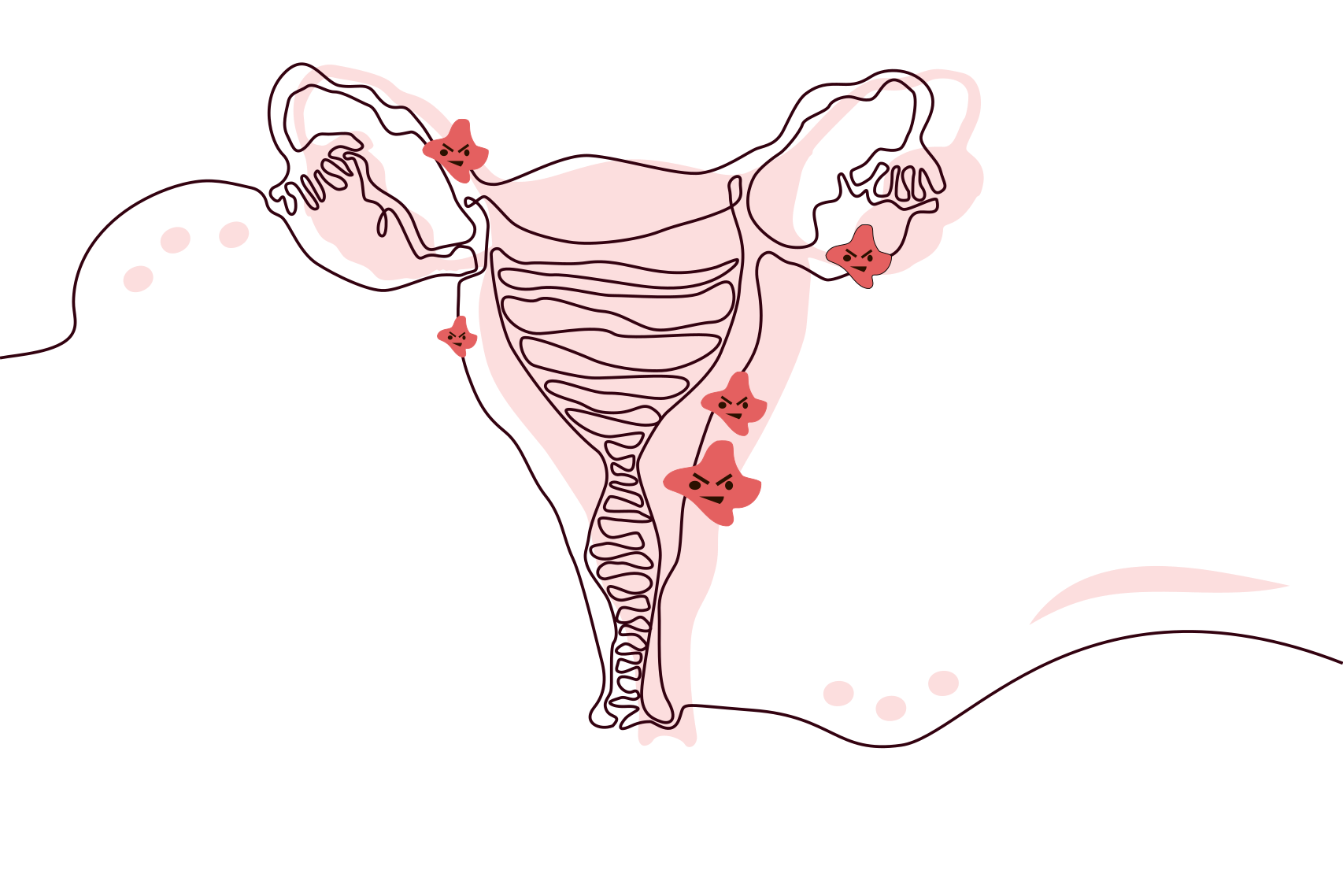
Was passiert im Körper
Endometriose tritt auf, wenn Zellen, die normalerweise die Gebärmutter auskleiden, an anderen Stellen im Körper wachsen. Dieses abnormale Wachstum kann starke Schmerzen, Entzündungen und sogar die Bildung von Narbengewebe verursachen. Die Schwere der Endometriose korreliert jedoch nicht immer mit dem Grad der erlebten Schmerzen. Einige Frauen mit schwerer Endometriose verspüren wenig bis keine Schmerzen, während andere mit einer milderen Form starke Schmerzen haben. Diese Inkonsistenz erschwert die Diagnose und Behandlung der Endometriose. Die genaue Ursache der Endometriose ist unbekannt. Es gibt jedoch verschiedene Theorien, wie die retrograde Menstruation, bei der Menstruationsblut mit Endometriumzellen durch die Eileiter zurück in die Bauchhöhle fließt, anstatt aus dem Körper. Andere vermuten, dass Hormone oder das Immunsystem eine Rolle spielen könnten.
Symptome: Die Anzeichen der Endometriose erkennen
Endometriose ist eine schwer zu diagnostizierende Erkrankung, die eine Vielzahl von Symptomen verursacht. Die häufigsten davon sind schmerzhafte Perioden, Beschwerden beim Geschlechtsverkehr, Schmerzen beim Wasserlassen und Beschwerden beim Stuhlgang. Frauen mit Endometriose können auch starke Blutungen während oder zwischen den Perioden erleben. Chronische Schmerzen im unteren Rücken und Becken außerhalb der Menstruation sowie starke Müdigkeit können ebenfalls häufige Anzeichen der Krankheit sein. Verdauungsprobleme wie Durchfall, Verstopfung, Blähungen und Übelkeit können besonders während der Menstruation auftreten. In einigen Fällen kann sich die Endometriose über die Fortpflanzungsorgane hinaus entwickeln. Sie kann in der Blase auftreten und Symptome wie häufiges Wasserlassen, einen starken Harndrang und Blut im Urin verursachen. Sie kann auch im Darm wachsen und Symptome wie Schmerzen beim Stuhlgang, Blutungen aus dem Rektum und anhaltende Verstopfung verursachen.
Fortschritte in der Diagnostik
Die Diagnose der Endometriose war lange Zeit eine medizinische Herausforderung. Lange Zeit war die Laparoskopie, ein chirurgisches Verfahren, das einzige definitive Diagnosewerkzeug. Neuere Entwicklungen in nicht-invasiven Diagnosemethoden, wie ein Speicheltest, zeigen jedoch vielversprechende Ergebnisse. Es ist wichtig zu beachten, dass Speicheltests zwar eine weniger invasive Methode bieten, aber weitere Forschung erforderlich ist, um die Genauigkeit und Implementierung zu verbessern.

Endometriose und Fruchtbarkeit
Etwa 30%-50% der Frauen mit Endometriose haben Schwierigkeiten, schwanger zu werden. Endometriose kann die Beckenanatomie einer Frau verzerren, und Entzündungen durch Endometriose können die Funktion von Spermien oder Eizellen negativ beeinflussen und den Empfängnisprozess erschweren. Viele Frauen mit leichter bis mittelschwerer Endometriose können jedoch trotzdem schwanger werden und eine Schwangerschaft bis zum Ende austragen. Ärzte raten Frauen mit Endometriose manchmal, das Kinderkriegen nicht zu lange hinauszuzögern, da sich die Erkrankung mit der Zeit verschlimmern kann.

Die Vor- und Nachteile der Hormontherapie
Die Behandlung der Endometriose hängt vom Ausmaß der Erkrankung, den Symptomen und davon ab, ob du schwanger werden möchtest. Hormontherapie ist oft eine Erstlinienbehandlung zur Linderung der Endometriose-Symptome. Diese Methode zielt darauf ab, die Hormonspiegel zu regulieren und somit das Wachstum von Endometriumgewebe zu kontrollieren. Hormonelle Verhütungsmittel, Gonadotropin-Releasing-Hormon (Gn-RH) Agonisten und Antagonisten, Gestagentherapie und Aromatasehemmer sind einige der verfügbaren Optionen. Hormontherapie ist jedoch keine Heilung, und die Symptome können nach Beendigung der Behandlung zurückkehren. Mögliche Nebenwirkungen wie Stimmungsschwankungen, Gewichtszunahme und Knochenschwund müssen ebenfalls berücksichtigt werden.
Eine Autoimmunverbindung?
Endometriose wird heute nicht als klassische Autoimmunerkrankung eingeordnet, aber das Immunsystem spielt eindeutig eine Rolle. Studien zeigen, dass Entzündungsprozesse, veränderte Immunantworten und eine gestörte Gewebeheilung dazu beitragen können, dass Endometrioseherde wachsen und bestehen bleiben.
Forscher:innen sprechen deshalb zunehmend von einer systemischen Erkrankung: nicht nur lokal im Becken, sondern mit Auswirkungen auf Schmerzverarbeitung, Immunbalance und Stoffwechsel. Was genau Ursache und was Folge ist, wird noch untersucht
Was bedeutet das für Betroffene?
Nicht, dass man „eine Autoimmunerkrankung hat“, sondern dass Immunsystem, Hormone und Nervensystem eng miteinander verbunden sind. Und genau hier entstehen neue Forschungsansätze für Diagnostik und Therapie.
Deinen Körper und Geist nähren
Die Behandlung der Endometriose erfordert einen umfassenden Ansatz, der Ernährung und Lebensstiländerungen einschließt. Die Bedeutung von Ernährung und Lebensstil wird im Kontext von Autoimmunerkrankungen noch wichtiger. Empfehlungen umfassen:
- Eine mediterrane Ernährung - Reich an Obst, Gemüse, Vollkornprodukten, magerem Eiweiß und gesunden Fetten.
- Brokkoli - Enthält Verbindungen, die helfen, Entzündungen zu reduzieren.
- Omega-3-Fettsäuren - Lebensmittel wie Lachs, Makrele, Sardinen, Leinöl und Walnüsse.
- Glutenfreie Alternativen - Produkte auf Basis von Linsen, Quinoa oder Mais.
- Eine histaminreduzierte Ernährung - Vermeide histaminreiche Lebensmittel wie Schokolade, Tomaten, Spinat, fermentiertes Gemüse, gereifte Käsesorten und gepökeltes Fleisch.
- Vermeide potenzielle entzündliche Auslöser - Lebensmittel wie Gluten, Eier und Milchprodukte.
- Regelmäßige Bewegung - Schwimmen, Wandern, alles, was sich gut anfühlt.
- Stressmanagement - Wie Achtsamkeit und Meditation.
Neben der Ernährung sind auch andere Lebensstiländerungen vorteilhaft.
Regelmäßige Bewegung kann helfen, Symptome zu lindern, sollte jedoch an individuelle Umstände angepasst werden, um eine Verschlimmerung der Symptome zu vermeiden. Stressmanagement ist entscheidend, da Stress Schübe bei Autoimmunerkrankungen auslösen kann. Techniken wie Achtsamkeit und Meditation können wertvoll sein, um den Geist zu beruhigen und eine ausgeglichene mentale und damit körperliche Gesundheit zu erhalten.
Caona Health: Frauen durch evidenzbasierte Lösungen stärken
Endometriose, obwohl herausfordernd und komplex, ist nicht unüberwindbar. Unser Wissen über diese Erkrankung entwickelt sich ständig weiter und eröffnet innovative Wege zur Diagnose und Behandlung. Die möglichen Verbindungen zur Autoimmunität deuten auf einen Paradigmenwechsel in unserem Verständnis der Endometriose hin und versprechen eine neue Welle therapeutischer Strategien. Bei Caona streben wir danach, diese wissenschaftlichen Erkenntnisse in praktische Lebensstil- und Ernährungsstrategien umzusetzen, die denen helfen können, die mit Erkrankungen wie Endometriose kämpfen. Unsere Mission ist es nicht nur zu unterstützen, sondern Frauen zu befähigen, ihre Gesundheit selbst in die Hand zu nehmen, indem wir gezielte und evidenzbasierte Lösungen anbieten. Denke daran, du bist auf dieser Reise nicht allein, und es ist in Ordnung, Unterstützung zu suchen. Wissen ist wirklich Macht, wenn es um Gesundheit geht.
Deine Endo-Lifestyle-Checkliste
- Diäten, die potenzielle entzündliche Auslöser wie Gluten, Eier und Milchprodukte ausschließen, können vorteilhaft sein.
- Erwäge eine mediterrane Ernährung: Diese Ernährung betont Obst, Gemüse, Vollkornprodukte, mageres Eiweiß und gesunde Fette, während verarbeitete Lebensmittel und Zucker eingeschränkt werden.
- Integriere Brokkoli in deine Ernährung: Brokkoli enthält Verbindungen, die helfen können, Entzündungen im Zusammenhang mit Endometriose zu reduzieren.
- Omega-3-Fettsäuren einbeziehen: Lebensmittel, die reich an Omega-3-Fettsäuren sind, wie fetter Fisch (Lachs, Makrele, Sardinen), Leinöl und Walnüsse, haben entzündungshemmende Eigenschaften, die bei der Behandlung von Endometriose-Symptomen hilfreich sein können.
- Die potenziellen Vorteile einer glutenfreien Ernährung erkunden: Einige Personen berichten von einer Verbesserung der Symptome nach dem Ausschluss von Gluten aus ihrer Ernährung, obwohl weitere Forschung erforderlich ist, um einen definitiven Zusammenhang zu etablieren.
- Eine histaminreduzierte Ernährung in Betracht ziehen: Histamine können zur Schmerzverstärkung beitragen, und einige Personen mit Endometriose können davon profitieren, histaminhaltige Lebensmittel wie Schokolade, Tomaten, Spinat, fermentiertes Gemüse, gereifte Käsesorten und gepökeltes Fleisch zu vermeiden
Quellen
- Mayo Clinic Staff. (n.d.). Endometriosis - Symptoms and causes. Mayo Clinic.
Retrieved from https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656 - Goldstein, S. R., Dun, E. C., & Casablanca, Y. (2023).
A non-invasive diagnostic tool for endometriosis based on the detection of menstrual blood contamination in urine. PubMed.
Retrieved from https://pubmed.ncbi.nlm.nih.gov/34117493/ - American College of Obstetricians and Gynecologists. (n.d.). Endometriosis. ACOG.
Retrieved from https://www.acog.org/womens-health/faqs/endometriosis - Parazzini, F., Vigano, P., Candiani, M., & Fedele, L. (2013). Diet and endometriosis - revisiting the link. PubMed.
Retrieved from https://pubmed.ncbi.nlm.nih.gov/24589191/ - Mayo Clinic Staff. (n.d.). Endometriosis - Diagnosis and treatment. Mayo Clinic.
Retrieved from https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661 - Fung, J. N., Montgomery, G. W., Girling, J. E., & Holdsworth-Carson, S. J. (2020). Endometriosis and autoimmunity: a systematic review. PubMed.
Retrieved from https://pubmed.ncbi.nlm.nih.gov/32896055/ - Harvard Health Publishing. (n.d.). Lifestyle Changes for Endometriosis. Harvard Health.
Retrieved from https://www.health.harvard.edu/diseases-and-conditions/lifestyle-changes-for-endometriosis - Pozza, C., Isensee, J., & Artati, A., et al. (2023). A saliva-based diagnostic miRNA signature for endometriosis. PubMed.
Retrieved from https://pubmed.ncbi.nlm.nih.gov/35160066/ - Riedl, M. (n.d.). Histaminunverträglichkeit: Therapie. NDR.
Retrieved from https://www.ndr.de/ratgeber/gesundheit/histaminunvertraeglichkeittherapie100.pdf - Norddeutscher Rundfunk. (n.d.). Omega-3-Fettsäuren: Warum sie gesund sind. NDR.
Retrieved from https://www.ndr.de/ratgeber/gesundheit/Omega-3-Fettsaeuren-Warum-sie-gesund-sind,fettsaeuren100.html - Yamaguchi, M., Araki, R., & Yoshimoto, S., et al. (2019). Broccoli sprout extract shows benefits for autoimmune, endometriosis patients. MDPI.
Retrieved from https://www.mdpi.com/1422-0067/21/24/9397 - Burney, R.O., & Giudice, L.C. (2012). Pathogenesis and pathophysiology of endometriosis. Fertil Steril.
Retrieved from https://pubmed.ncbi.nlm.nih.gov/22819185/ - Nezhat, C., Li, A., & Falik, R., et al. (2018). Bowel endometriosis: diagnosis and management. Am J Obstet Gynecol.
Retrieved from https://pubmed.ncbi.nlm.nih.gov/29273494/ - Shigesi N, Kvaskoff M, Kirtley S, Feng Q, Fang H, Knight JC, Missmer SA, Rahmioglu N, Zondervan KT, Becker CM. The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Hum Reprod Update. 2019 Jul 1;25(4):486-503. doi: 10.1093/humupd/dmz014. PMID: 31260048; PMCID: PMC6601386.
Retrieved from https://pubmed.ncbi.nlm.nih.gov/31260048/

.jpg)


